The Neuropathology Department at Heidelberg University Hospital led by Professor Andreas von Deimling, have developed a new computer-based method. “We hope that our new molecular classification method will help improve diagnostic accuracy in CNS tumors and, thus, also improve the chances for successful treatment,” said von Deimling.
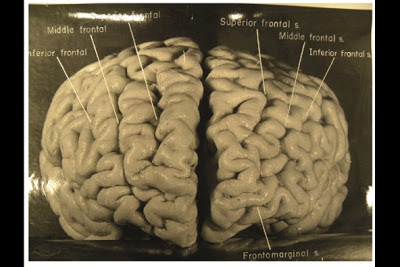
The researchers analyzed specific DNA methylations. Different cell types exhibit characteristic patterns of DNA methylation which enable scientists to draw conclusions about a tumor’s cellular origin. "We have developed computer-based algorithms that reliably differentiate 82 types of CNS tumors based on their methylation patterns," said Professor David Capper, who is one of the four first authors of the study. “Particularly in tumors which we cannot easily assign to a diagnostic category based solely on microscopic examination, methylation analysis is often helpful to make a precise diagnosis. The analysis of approximately 2,800 reference tumor samples additionally made it possible to classify tumors into specific subgroups that are not yet included in the classifications that have been used so far.”
In order to test whether the method is suitable for use in clinical routine diagnostics, the scientists analyzed more than 1,100 additional tumor samples. In about twelve percent of the cases, they were able to correct the initial diagnosis using the methylation patterns. In almost all cases where it was possible, further molecular-diagnostic examinations showed that molecular classification characterized the tumors even better than the initial microscopic diagnosis.
“We are convinced that our new method is well suited to be used in the clinic,” said Stefan Pfister, one of the paper's authors. He added: “We have made our classification system available online in order to enable researchers to analyze their data at our platform.”
Reference: Capper, D., Jones, D. T. W., Sill, M., Hovestadt, V., Schrimpf, D., Sturm, D., … Pfister, S. M. (2018). DNA methylation-based classification of central nervous system tumours. Nature. https://doi.org/10.1038/nature26000