Comments are encouraged!!!!
Clinical
History
1. Gender of patient: __male
___female
2. Age at presentation: _
_ years _ _ months
3. Age at biopsy: _ _ years _ _ months
4. Symptoms at presentation (check all that
apply):
Weakness
Hypotonia
Muscle pain
Cardiac
disease
Central
nervous system disease
Respiratory
difficulties
Contractures
Failure to
thrive
Others (see
item 8)
5. Elevated
creatine kinase: Yes No Unknown _______
Patient Value _________(Normal Range)
6. Familial
Inheritance:____None ___Autosomal Recessive ____Autosomal Dominant ____X-linked
7. EMG
Findings:
____Not known ____Myopathic ____Neuropathic
8. Other
symptoms, signs, and lab data: ____________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________
Muscle Biopsy Tissue
Information
1.
Name of Muscle:___________________________________________________________________
2.
Size of tissue collected*: ______
X ______ X
______ cm
3.
Date of tissue collection*: __ __ / __ __ / __ __ __ __
m m
d d y
y y y
4.
Biopsy method: Open Needle
5.
Freezing or Fixation Used*? Frozen: Amount: _____ mg Not known
Formalin-fixed: Amount: _____ mg Not known
Paraffin-embedded: Amount: _____ mg Not known
Epon-embedded: Amount: _____ mg Not known
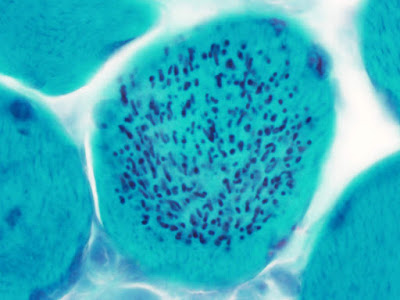
Histological
Findings in Muscle Biopsy or Autopsy specimens
1. Which
standard histochemical stains were used*? (choose all that apply)
H and E Gomori
trichrome NADH COX SDH
COX/SDH PAS Oil Red O ATPase 4.3 ATPase 4.6
ATPase 9.4 Other,
specify: __________________________________________________________________________________________________________________________________________________________________________________
2. Which
of the following diagnostic abnormalities were noted on histochemical stains
(choose all that apply)*?
Fatty replacement ___absent ___mild ___moderate ___severe
Endomysial fibrosis ___absent ___mild ___moderate ___severe
Myofiber degeneration ___absent ___mild ___moderate ___severe
Necrosis ___absent ___mild ___moderate ___severe
Myophagocytosis ___absent ___present in ____ fibers
Myofiber regeneration
(Basophilic fibers) ____absent ___present in _____ fibers
Abnormalities
of fiber type ____absent _____present
Specify*: Type 1
predominance ______ % Type 1 fibers
Type 2
predominance ______% Type 2 fibers
Fiber type
grouping (of both fiber types)
Hypertrophic fibers ____absent _____present in _____ fibers
Atrophy/Hypotrophy ____absent _____present
Specify: All fibers
within the specimen
Subsets of
fibers, leading to excessive variation in fiber size
Specify (choose all that
apply): Single
fibers Groups of
fibers
Type 1
fibers only Type 2
fibers only
Perifascicular distribution
Atrophic/hypotrophic fiber shape
Angulated Round
Myopathy-associated
pathological structures, specify:
Central nuclei _____absent _____present
Specify estimated % of fibers
(include eccentric nuclei): _____
Internal nuclei _____absent _____present
Specify estimated % of fibers
(if not quantified above): _____
Inclusion bodies ____absent ____present in _____ fibers
Rimmed vacuoles ____absent ____present in _____ fibers
Nemaline rods ____absent ____present
Specify: Restricted
to one fiber type, specify which: _____
Nuclear
rods present
Ragged red fibers ____absent ____present in _____fibers
COX- negative fibers Estimated number ______
Strongly SDH-reactive blood
vessels (SSV’s) _____absent _____present
Central cores ____absent ____present in _____ fibers
Minicores ____absent ____present
in ____ fibers
Core-like lesions ____absent ____present in ____ fibers
Targetoid fibers ____absent ____present in ____ % of fibers
Marked hypotrophy of type 1 fibers ____absent ____present
Inflammation ___absent ___mild ___moderate ___severe
Specify:
Distribution
Perivascular
Evidence of
vascular damage Thrombi
identified in blood vessels
Focal
Diffuse
Endomysial
Perimysial
Involving
fascia
Associated
with myofiber damage
Associated
with non-necrotic myofiber
Granulomas
Necrotizing
Non-necrotizing
Giant cells present Foreign
material present
Inflammatory cells identified
Specify (choose all that
apply):
Lymphocytes
Neutrophils
Macrophages
Eosinophils
(as a prominent component)
Microorganisms identified, specify which:
_________________________________________
Abnormal
storage material
Specify:
Excessive glycogen ____absent ____mild ____severe
Excessive intracellular
lipid ____absent ____mild ____severe
Additional
observations
____________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________
3. Which
immunohistochemical stains were used? (choose all that apply)
Myosin
immunohistochemistry (for fast and slow fibers)
Dystrophin
panel
Specify:
Dystrophin (DYS1) ____absent ____reduced ____normal
Dystrophin (DYS2) ____absent ____reduced ____normal
Dystrophin (DYS3) ____absent ____reduced ____normal
Dystrophin (BMD Hotspot) ____absent ____reduced ____normal
Spectrin ____absent ____reduced ____normal
Utrophin ____absent ____normal ____increased
Other
stains for limb-girdle or congenital muscular dystrophy
Specify:
Laminin a2/Merosin ____absent ____reduced ____normal
Alpha dystroglycan (VIA) ____absent ____reduced ____normal
Alpha dystroglycan (IIH) ____absent ____reduced ____normal
Beta dystroglycan ____absent ____reduced ____normal
Alpha sarcoglycan ____absent ____reduced ____normal
Beta sarcoglycan ____absent ____reduced ____normal
Delta sarcoglycan ____absent ____reduced ____normal
Gamma sarcoglycan ____absent ____reduced ____normal
Dysferlin ____absent ____reduced ____normal
Emerin ____absent ____reduced ____normal
Collagen VI ____absent ____reduced ____normal
Caveolin 3 ____absent ____reduced ____normal
Desmin ____absent ____reduced ____normal
Integrin a7 ____absent ____reduced ____normal
nNOS ____absent ____reduced ____normal
Inflammatory myopathy panel
CD4 ____absent ____present in ___ % of lymphocytes
CD8 ____absent ____present in ___ % of lymphocytes
CD20 ____absent ____present in ___ % of lymphocytes
CD45 ____absent ____present in ____% of mononuclear cells
CD68 ____absent ____present in ____% of mononuclear cells
C5b-9 ____absent ____present on endomysial capillary walls
Major Histocompatability
Complex ____absent ____sarcolemmal ____diffuse
4. Additional immunohistochemical/immunofluorescence
assays performed:
__________________________________________________________________________________
5. Other
abnormalities noted on immunohistochemistry: __________________________________
Epon-Embedded
Tissue/Electron Microscopy (Muscle Biopsy/Autopsy Specimens)
1. Abnormalities
seen on: Light
microscopy (Toluidine blue staining) Electron
microscopy
Both –
Light microscopy and Electron microscopy
2. Abnormalities
noted in: Contractile
apparatus
Sarcotubular organization
Mitochondria, specify (choose all that apply):
Abnormal
shape
Abnormal
numbers
Abnormal
location
Abnormal
architecture
3. Describe
any pathological inclusions noted: N/A
_________________________________________________________________________________________
_________________________________________________________________________________________
4. Describe
any abnormal storage material identified: N/A
_________________________________________________________________________________________
_________________________________________________________________________________________
Interpretation:
Comment: