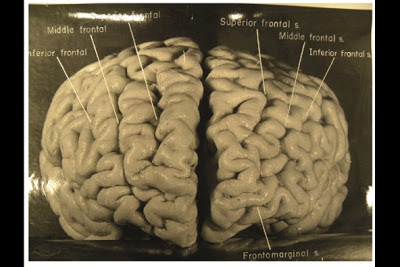
Photographs taken shortly after his death, but never before analysed in
detail, have now revealed that Einstein’s brain had several unusual
features, providing clues about the neural basis of his
extraordinary mental abilities.
Nature.com reports that, while doing Einstein's autopsy, the pathologist Thomas Harvey removed
the physicist's brain and preserved it in formalin. He then took dozens
of black and white photographs of it before it was cut up into 240
blocks. Now, anthropologist Dean Falk of Florida State University in
Tallahassee and her colleagues have obtained 12 of Harvey’s original
photographs from the National Museum of Health and Medicine in Silver
Spring, Maryland, analysed them and compared the patterns of convoluted
ridges and furrows with those of 85 brains described in other studies.Many of the photographs were taken from unusual angles,
and show structures that were not visible in photographs that have been
analysed previously. The analysis was recently published today in the journal Brain. The most striking observation, says Falk, was “the
complexity and pattern of convolutions on certain parts of Einstein's
cerebral cortex”, especially in the prefrontal cortex, and also parietal
lobes and visual cortex.
I discuss issues pertaining to the practice of neuropathology -- including nervous system tumors, neuroanatomy, neurodegenerative disease, muscle and nerve disorders, ophthalmologic pathology, neuro trivia, neuropathology gossip, job listings and anything else that might be of interest to a blue-collar neuropathologist.
Wednesday, November 21, 2012
Thursday, November 15, 2012
CAP seeking input on revised brain/spinal cord tumor protocol
 Prior to the release of the revised Brain/Spinal Cord Protocol, the College
of American Pathologists (CAP) will host a public comment period. You can review
the revisions and submit feedback online. The public comment period will
run through November 30, 2012. Please note that comments are not instantly
available for review and will be posted on a weekly basis.
Prior to the release of the revised Brain/Spinal Cord Protocol, the College
of American Pathologists (CAP) will host a public comment period. You can review
the revisions and submit feedback online. The public comment period will
run through November 30, 2012. Please note that comments are not instantly
available for review and will be posted on a weekly basis.
Tuesday, November 13, 2012
Review Article: "Thinking and Talking About Life Expectancy in Incurable Cancer"
As a follow-up to my previous post, here's a perspective from a June 2011 article in Seminars in Oncology:
"Most patients with incurable cancer want information about the impact cancer will have on their future, and many want specific estimates of the most likely, best case, and worst case scenarios for survival. With improved understanding of life expectancy, patients are better equipped to make appropriate treatment decisions and plans for the future. Although physicians acknowledge that patients with incurable cancer want prognostic information and benefit from this, most struggle to provide it and experience difficulty in making reliable estimates, communicating them, and tailoring the information to the individual patient."
"Most patients with incurable cancer want information about the impact cancer will have on their future, and many want specific estimates of the most likely, best case, and worst case scenarios for survival. With improved understanding of life expectancy, patients are better equipped to make appropriate treatment decisions and plans for the future. Although physicians acknowledge that patients with incurable cancer want prognostic information and benefit from this, most struggle to provide it and experience difficulty in making reliable estimates, communicating them, and tailoring the information to the individual patient."
Thursday, November 8, 2012
Why genetically profile a glioma?
A couple of weeks ago I met with representatives of Castle Biosciences regarding their proprietary gene expression profile assay for glioblastomas, called DecisionDx-GBM, as well as their multi-methylation test for grade II and III gliomas, called DecisionDX-G-CIMP. During the meeting, I brought up a crucial issue raised by a Neuropathology Blog reader. I'll quote part of the reader's comment: "I doubt anyone wants to give a patient a life expectancy prediction
based on the results of this test, since individuals may fall at any
point on a survival curve. So I would not be eager to recommend this
test until there are alternative treatments for those in poor prognosis
groups." The representative's response to this concern was that prognostication is an important part of the decision-making process that a neuro-oncologist, in collaboration with the patient, takes into account in recommending a course of treatment. For example, when should Avastin be introduced into the regimen? If a patient has a tumor with a genetic signature that has a longer median survival, perhaps the neuro-oncologist would be more likely to hold back on the introduction of Avastin, keeping it in his armamentarium for later in the disease course. I would add that if I personally had the misfortune of being diagnosed with a glioblastoma, I would like to have as much prognostic information as possible just to help me adjust psychologically to dealing with the the disease. I realize that one individual can fall at any point on a survival curve. But put yourself in the patient's shoes for a moment. Wouldn't you want this test done, as well as IDH1 mutation, MGMT methylation status, 1p/19q testing, and whatever else that might be available to get as much information as possible about this disease has invaded you? Since, as Castle Biosciences states, insurance will cover this test, I see both practical and intangible benefits to doing it. I would be curious to hear what other neuropathologists have to say about this issue in general and about the Castle Biosciences tests in particular. I should note that the Castle tests were developed by the widely-respected neuropathologists Dr. Kenneth Aldape at MD Anderson. I am seriously entertaining the idea of routinely using the Castle Biosciences tests at my institution and would be interested in the advice of the neuropathology community as a whole regarding this issue. Please post to comments.
Tuesday, November 6, 2012
Best Post of May 2012: New Study Looks at Head Impacts in Youth Football
The next in our "Best of the Month" series is from May 14, 2012:
We neuropathologists, and society as a whole, have spent a lot of time over the last couple of years rethinking the long-term effects of repeated concussive and subconcussive blows to the heads of professional and college football players. But what about the 3.5 million kids in American who play below the high school level? Dr. Peter Cummings today sent me a link to a report regarding groundbreaking research being done at Virginia Tech in which impact-measurement instruments were placed on 7 and 8-year-old football players. Data was collected on more than 750 hits to the head over the course of the season.
Lead researcher, Stefan Duma, a professor of Biomedical Engineering, reports that some head impacts in youth football are equal in force to some of the bigger hits he sees at the college level. The average kid received 107 head impacts during the course of the season. This is fewer than seen in high school (which averages about 500 per season) and college (which amounts to about 1000 per season.). But what about the magnitude of these hits? The median impact was 15 g's. In Duma's study, there were 38 impacts that were 40 g or greater (almost all of which occurred during practice). Six impacts were over 80 g's, which starts to get into the range of risk for concussion. “Nobody expected to see hits of this magnitude,” says Duma, who speculates that once players start seeing hits of 30 g's or above, there is a risk for cumulative injury.
Here's the video report from reporter Stone Philips. The interviews with the parents of these youth players perplexed me. All of the parents featured found the results concerning, but none expressed any thoughts about having their child switch to another sport.
We neuropathologists, and society as a whole, have spent a lot of time over the last couple of years rethinking the long-term effects of repeated concussive and subconcussive blows to the heads of professional and college football players. But what about the 3.5 million kids in American who play below the high school level? Dr. Peter Cummings today sent me a link to a report regarding groundbreaking research being done at Virginia Tech in which impact-measurement instruments were placed on 7 and 8-year-old football players. Data was collected on more than 750 hits to the head over the course of the season.
Lead researcher, Stefan Duma, a professor of Biomedical Engineering, reports that some head impacts in youth football are equal in force to some of the bigger hits he sees at the college level. The average kid received 107 head impacts during the course of the season. This is fewer than seen in high school (which averages about 500 per season) and college (which amounts to about 1000 per season.). But what about the magnitude of these hits? The median impact was 15 g's. In Duma's study, there were 38 impacts that were 40 g or greater (almost all of which occurred during practice). Six impacts were over 80 g's, which starts to get into the range of risk for concussion. “Nobody expected to see hits of this magnitude,” says Duma, who speculates that once players start seeing hits of 30 g's or above, there is a risk for cumulative injury.
Here's the video report from reporter Stone Philips. The interviews with the parents of these youth players perplexed me. All of the parents featured found the results concerning, but none expressed any thoughts about having their child switch to another sport.
Thursday, November 1, 2012
Robert Scully Has Died
A message just received from neuropathologist David Louis, Pathologist-in-Chief at Massachusetts General Hospital:
 |
| Dr. Robert E. Scully |
Dear colleagues,
It is with deep sadness that I let you know that our dear
friend, mentor and colleague, Dr. Robert E. Scully, passed away late yesterday
afternoon [October 30] at the age of 91.
Dr. Scully was a giant in the field of pathology who
devoted almost all of his career to the Mass. General Hospital. He was on the
active staff for 55 years and stepped down from active practice only in the
past decade. After graduating from Harvard Medical School in 1944, he trained
at the Peter Bent Brigham Hospital and then joined our staff in the early
1950s. Dr. Scully rapidly became known as a peerless diagnostic pathologist.
Although he soon became recognized around the world for special expertise in
gynecologic and testicular pathology, his opinion was sought in nearly all
areas of pathology by colleague after colleague for many decades here at MGH
and elsewhere. He contributed over 480 papers to the literature and described
many hitherto unrecognized entities, largely in gynecologic pathology but also
to a significant degree in testicular pathology. His book on the ovary was
considered the standard reference work on the subject and the current
classification of gynecologic tumors derives largely from his work. Dr. Scully
was also the Editor of the Case Records of the Massachusetts General Hospital
in New England Journal of Medicine for a remarkable 27 years. He was an
Emeritus Professor of Pathology at Harvard Medical School.
Dr. Scully was also a gentleman and a gentle man. He was
quiet but firm, honest, careful, considerate and happy to give credit to
others. As such, he was a beloved figure in the field of pathology worldwide.
Subscribe to:
Comments (Atom)
Neuropathology Blog is Signing Off
Neuropathology Blog has run its course. It's been a fantastic experience authoring this blog over many years. The blog has been a source...
-
Neuropathology Blog has run its course. It's been a fantastic experience authoring this blog over many years. The blog has been a source...
-
A neuropathology colleague in Toronto (Dr. Phedias Diamandis) is developing some amazing AI-based tools for pathology and academia. He hel...