Thanks, Dr. McLendon, for pointing out this helpful website.
I discuss issues pertaining to the practice of neuropathology -- including nervous system tumors, neuroanatomy, neurodegenerative disease, muscle and nerve disorders, ophthalmologic pathology, neuro trivia, neuropathology gossip, job listings and anything else that might be of interest to a blue-collar neuropathologist.
Wednesday, June 29, 2011
Looking for pictures? PathologyPics.com has plenty
Dr. Roger E. McLendon called my attention to PathologyPics.com a very good, pictorially-oriented general pathology website which includes many examples of both classic and rare brain tumors. Here, for example, is an example from the site of a chordoid glioma of the third ventricle:
Thursday, June 23, 2011
I have discovered my ApoE status
I just got my ApoE results back from 23andMe.com. When I ordered the test, the first question I posed to readers was whether it was wise to even find out whether or not I have the epsilon 4 allele. One commentator, "Agent 86", quoted the ancient Greek philosopher Epictetus for guidance on this issue. In 135 AD, Epictetus argued that one should emotionally separate oneself from those things which are not one's own -- i.e., those things over which one has no control. Therefore, had he known what a gene was at the time, Epictetus would have counted one's genome as among those things that is not one's own. As such, knowing his ApoE status would have been of no consequence either way to Epictetus. I do find it rather easy to take this Epictetusian attitude toward my ApoE status. But because I find it exceedingly difficult to adopt this attitude of separateness toward many other things in my life over which I have no control, I can certainly understand how others could feel emotionally affected by knowledge of their own ApoE status.
I then had a second question: Should I make my ApoE results public? I was surprised by the number of people who recommended against doing so. The main objection seemed to be the potential that an insurance company might refuse to cover me if it were known that I was at increased risk for the development of Alzheimer's disease. I agree with one commentator who stated that this is a "worst-case scenario" and continually worrying about worst-case scenarios is not a wise way to live one's life. I might also add that it might be in an insurance company's best interest for me to get Alzheimer's disease at a relatively earlier age (in my 60's rather than in my 80's) as I would likely die at a younger age and thereby cost the company less money over the long run. That being said, in deference to all those who weighed in on this matter, I have elected not to publicly share my ApoE status. I appreciate all those who engaged in this discussion; and I suspect that this kind of discussion will be ongoing in many circles in the decades to come as personalized medicine, based on genomic profiling, emerges in the new age of theragnostics.
I then had a second question: Should I make my ApoE results public? I was surprised by the number of people who recommended against doing so. The main objection seemed to be the potential that an insurance company might refuse to cover me if it were known that I was at increased risk for the development of Alzheimer's disease. I agree with one commentator who stated that this is a "worst-case scenario" and continually worrying about worst-case scenarios is not a wise way to live one's life. I might also add that it might be in an insurance company's best interest for me to get Alzheimer's disease at a relatively earlier age (in my 60's rather than in my 80's) as I would likely die at a younger age and thereby cost the company less money over the long run. That being said, in deference to all those who weighed in on this matter, I have elected not to publicly share my ApoE status. I appreciate all those who engaged in this discussion; and I suspect that this kind of discussion will be ongoing in many circles in the decades to come as personalized medicine, based on genomic profiling, emerges in the new age of theragnostics.
Tuesday, June 21, 2011
What's wrong with finding out and releasing my ApoE status?
In a recent blog post, I stated that I intended to publish my ApoE status on the blog when I get the results back from 23andMe.com. I was surprised to find that some people objected to this. One associate said that by publishing information about my genetic status, I would be "normalizing" the dissemination of information that should be confidential. That sets a bad precedent for the use of personal genomic data. Another individual emailed me the following suggestion: "Instead of posting your results, maybe you would consider instead the value of not doing so at the request of an 'anonymous' reader and keeping the information private in order to stimulate debate about finding out about a disease process for which there is no cure." Finally, "jd" commented in the original post about the wisdom of getting the test done at all: "Why would you do that? If you come back 4/4 or 3/4, that'll be hanging over you the rest of your life. If there were a cure for Alzheimer's, that'd be different."
Tuesday, June 14, 2011
A 58-year-old woman presenting with headache and unsteadiness of gait
Here's a recent case of mine involving a lesion in the third ventricle of a 58-year-old woman who presented with headache and unsteadiness of gait. First, the imaging:
The neuroradiologist thought perhaps the lesion was a craniopharyngioma. But, the neurosurgeon was surprised that the lesion seemed to "pop out". Here's the specimen I received:
I smeared some of the viscous fluid from the cut surface onto a glass slide, cover-slipped it, and viewed it under polarized light:
Those cholesterol crystals certainly seem to suggest the possibility of craniopharyngioma. But, craniopharyngiomas do not have a smooth outer surface and do not just "pop out" into the neurosurgeon's hand. Here was my first glimpse of the histology the next day:
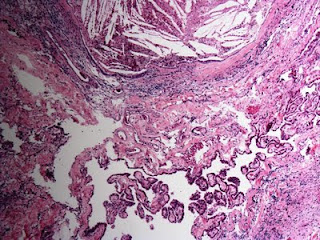
Cholesterol clefts and giant cells. Note in the upper picture that this xanthogranulomatous reaction appears to be continuous with the choroid plexus. Could this be a xanthogranuloma of the choroid plexus? I considered that, until I looked elsewhere on the slide and saw this:
This is the ciliated epithelium characteristic of a colloid cyst of the third ventricle, a tumor that can indeed "pop out" into the neurosurgeon's hand. Gross inspection did not reveal a cyst per se because the exuberant xanthogranulomatous reaction obliterated it. Cases like this have been described in the literature. For example, Dr. David Louis and colleagues wrote in a 1994 article entitled Third ventricle xanthogranulomas clinically and radiologically mimicking colloid cysts: Report of two cases (Journal of Neurosurgery. 81(4):605-9, 1994 Oct.) that "histopathologic examination revealed xanthogranulomas of the choroid plexus with only microscopic foci of colloid cyst-like structures." I would argue quite the opposite: that the xanthogranuloma derived from the colloid cyst and extended into the choroid plexus. Indeed, Dr. Peter Burger and colleagues write in the fourth edition of Surgical Pathology of the Nervous System and Its Coverings that "a xanthogranulomatous reaction occasionally supervenes in colloid cysts, largely replacing the epithelium in some cases."
Cool case.
 | |
| Axial CT |
 |
| Sagittal T1 MRI |
 |
| Axial T2 MRI |
 |
| Coronal Gradient Echo |
 |
| Outer Surface |
 |
| Cut Surface |
Those cholesterol crystals certainly seem to suggest the possibility of craniopharyngioma. But, craniopharyngiomas do not have a smooth outer surface and do not just "pop out" into the neurosurgeon's hand. Here was my first glimpse of the histology the next day:
Cholesterol clefts and giant cells. Note in the upper picture that this xanthogranulomatous reaction appears to be continuous with the choroid plexus. Could this be a xanthogranuloma of the choroid plexus? I considered that, until I looked elsewhere on the slide and saw this:
This is the ciliated epithelium characteristic of a colloid cyst of the third ventricle, a tumor that can indeed "pop out" into the neurosurgeon's hand. Gross inspection did not reveal a cyst per se because the exuberant xanthogranulomatous reaction obliterated it. Cases like this have been described in the literature. For example, Dr. David Louis and colleagues wrote in a 1994 article entitled Third ventricle xanthogranulomas clinically and radiologically mimicking colloid cysts: Report of two cases (Journal of Neurosurgery. 81(4):605-9, 1994 Oct.) that "histopathologic examination revealed xanthogranulomas of the choroid plexus with only microscopic foci of colloid cyst-like structures." I would argue quite the opposite: that the xanthogranuloma derived from the colloid cyst and extended into the choroid plexus. Indeed, Dr. Peter Burger and colleagues write in the fourth edition of Surgical Pathology of the Nervous System and Its Coverings that "a xanthogranulomatous reaction occasionally supervenes in colloid cysts, largely replacing the epithelium in some cases."
Cool case.
Tuesday, June 7, 2011
The Link Between ApoE4 and Chronic Traumatic Encephalopathy appears to be weakening
 |
| Dr. Robert Cantu |
(Reference: Katsnelson A, Gene tests for brain injury still far from the football field. Nature Medicine. June 2011. 17:6, p. 638)
Monday, June 6, 2011
American Brain Banking Network renamed the International Brain Banking Network, with new website
 |
| Piotr B. Kozlowski, MD, PhD |
From Dr. Piotr B. Kozlowski, Touro College of Osteopathic Medicine, New York City:
"The website of the brain banking network formerly known as the American Brain Banking Network (ABBN), is now renamed as the International Brain Banking Network and its website can be found at http://www.intbbn.org/
"Please have a look at this website, still in a nascent state, and if the information regarding your brain/tissue bank needs to be updated, please let me know."
Subscribe to:
Comments (Atom)
Neuropathology Blog is Signing Off
Neuropathology Blog has run its course. It's been a fantastic experience authoring this blog over many years. The blog has been a source...
-
Neuropathology Blog has run its course. It's been a fantastic experience authoring this blog over many years. The blog has been a source...
-
A neuropathology colleague in Toronto (Dr. Phedias Diamandis) is developing some amazing AI-based tools for pathology and academia. He hel...